INDICATION
Abatacept is indicated in adult patients for the treatment of moderately-to-severely active rheumatoid arthritis and for the treatment of active psoriatic arthritis.
In patients two years of age and older, abatacept is also indicated for the treatment of moderately-to-severely active juvenile idiopathic arthritis.
Abatacept is also indicated for the prophylaxis of acute graft-versus-host disease, in combination with methotrexate.
And a calcineurin inhibitor such as tacrolimus, in patients two years of age and older who are undergoing hematopoietic stem cell transplantation from a matched or 1 allele-mismatched unrelated donor.
DRUG Doses
Adult and pediatric dosage
Injection, lyophilized powder for reconstitution (250mg/vial)
Solution for SC injection
- 125mg/mL prefilled syringe
- 125mg/mL autoinjector (Note: autoinjector has not been studied in patients aged below 18 years)
Rheumatoid Arthritis
Adult dosage (IV infusion)
- Weight below 60 kg: 500 mg
- Weight between 60-100 kg: 750 mg
- Weight above 100 kg: 1000 mg
Maintenance: Above dose repeated every 2 weeks two times, then every 4 weeks
SC injection
SC administration may be initiated with or without an IV loading dose
If an IV loading dose is used, administer the first SC injection within 1 day of infusion
125 mg SC every week
Transitioning from IV to SC: Administer the first SC dose instead of the scheduled IV dose
Psoriatic arthritis
Adult dosage (IV infusion)
- Weight below 60 kg: 500 mg
- Weight between 60-100 kg: 750 mg
- Weight above 100 kg: 1000 mg
Maintenance: Above dose repeated every 2 weeks for two times, then every 4 weeks
SC injection
125 mg SC every week without the need for an IV loading dose
Switching from IV to SC: Administer the first SC dose instead of the next scheduled IV dose
Graft versus Host Disease
Adult dosage
- Day -1 (day before transplantation): 10 mg/kg IV (up to 1,000 mg) IV, followed by
- Days 5, 14, and 28 (after transplantation): 10 mg/kg IV (up to 1,000 mg) IV
Pediatric dosage
- Aged less than 2 years: Safety and efficacy not established
Aged 2 to 5 years
- Day -1 (day before transplantation): 15 mg/kg IV, followed by
- Days 5, 14, and 28 (after transplantation): 12 mg/kg IV
Aged above 6 years
- Day -1 (day before transplantation): 10 mg/kg IV (up to 1,000 mg) IV, followed by
- Days 5, 14, and 28 (after transplantation): 10 mg/kg IV (up to 1,000 mg) IV
Juvenile idiopathic arthritis
Pediatric dosage (IV infusion)
- Aged below 6 years: Safety and efficacy not established
- Aged above 6 years old and weight below 75 kg: Loading dose of 10 mg/kg IV over 30 minutes
Maintenance: Same dose repeated 2 and 4 weeks after the loading dose, THEN every 4 weeks
Weight above 75 kg: Administer as in adult
SC administration
- Aged below 2 years: Safety and efficacy not established
- Aged above 2 years
- Weight between 10 to 24 kg: 50 mg SC once weekly
- Weight between 25 to 49kg: 87.5 mg SC once weekly
- Weight above 50 kg: 125 mg SC once weekly
- Administer without a loading dose
Administration
None
Contraindications
- Inactive tuberculosis.
- A bad infection.
- Cancer or malignancy.
- A reduction in the body’s resistance to infection.
- Chronic obstructive pulmonary disease.
Side effects:
Common side effects of Abatacept include:
Fever, nausea, diarrhea, stomach pain, headache, and cold symptoms (stuffy nose, sneezing, sore throat, cough)
Serious side effects of Abatacept include:
Fever, chills, night sweats, flu symptoms, weight loss, feeling very tired, dry cough, sore throat, warmth, pain, or redness of your skin, trouble breathing, stabbing chest pain, wheezing, cough with yellow or green mucus, pain or burning while urinating, and signs of skin infection such as itching, swelling, warmth, redness, or oozing
Rare side effects of Abatacept include:
None
This is not a complete list of side effects and other serious side effects or health problems that may occur as a result of the use of this drug. Call your doctor for medical advice about serious side effects or adverse reactions. You may report side effects or health problems to FDA at 1-800-FDA-1088.
Precaution & Warnings
- Appropriate medical support measures for the treatment of hypersensitivity reactions should be available for immediate use in event of reaction; if an anaphylactic or other serious allergic reaction occurs, stop administration immediately; institute appropriate therapy; permanently discontinue therapy.
- Higher risk for serious infections; concomitant use with a TNF antagonist can also increase the risk of infections and serious infections; concurrent therapy with another TNF antagonist is not recommended; discontinue if serious infections develop.
- Serious infections, including sepsis and pneumonia, are reported; some of these infections have been fatal; many of the serious infections have occurred in patients on concomitant immunosuppressive therapy which in addition to their underlying disease, could further predispose them to infection; a higher rate of serious infections has been observed in adult RA patients treated with concurrent TNF antagonists.
- Healthcare providers should exercise caution when considering therapy in patients with a history of recurrent infections, underlying conditions which may predispose them to infections, or chronic, latent, or localized infections; patients who develop a new infection while undergoing treatment should be monitored closely; administration should be discontinued if a patient develops a serious infection.
- Antirheumatic therapies have been associated with hepatitis B reactivation; screening for viral hepatitis should be performed following published guidelines before starting therapy.
- Before initiating therapy, patients should be screened for latent tuberculosis (TB) infection with a tuberculin skin test; therapy has not been studied in patients with a positive TB screen; safety of therapy in individuals with latent TB infection is unknown; patients testing positive in TB screening should be treated by standard medical practice before therapy.
- Before initiating therapy, update vaccinations following current vaccination guidelines; treated patients may receive current non-live vaccines; live vaccines should not be given concurrently or within 3 months after discontinuation; no data are available on the secondary transmission of infection from persons receiving live vaccines to patients receiving therapy; based on mechanism of action, therapy may blunt the effectiveness of some immunizations.
- Increased risk of lymphoma and lung cancer reported; significance unknown; increased risk of lymphoma associated with rheumatoid arthritis.
- Patients receiving therapy for RA reported developing adverse events more frequently, including COPD exacerbations, cough, rhonchi, and dyspnea; therapy in patients with COPD should be undertaken with caution and such patients should be monitored for worsening their respiratory status.
- The possibility exists for drugs inhibiting T cell activation, to affect host defenses against infections and malignancies since T cells mediate cellular immune responses; there have been reports of malignancies, including skin cancer in patients receiving therapy; periodic skin examinations are recommended for all treated patients, particularly those with risk factors for skin cancer.
- Higher incidence of infections and malignancy reported in the elderly; use caution.
Cytomegalovirus (CMV) and Epstein-Barr virus (EBV) reactivation
- CMV and EBV reactivation was reported in aGVHD prophylaxis after hematopoietic cell transplant (HSCT).
- Post-transplant lymphoproliferative disorder (PTLD) occurred in patients who received the drug for aGVHD prophylaxis during unrelated HSCT; all the PTLD events were associated with Epstein-Barr virus (EBV) infection; monitor patients for EBV reactivation following institutional practices; provide prophylaxis for EBV infection for 6 months post-transplantation to prevent EBV-associated PTLD.
- Cytomegalovirus (CMV) invasive disease reported in patients who received therapy for aGVHD prophylaxis during unrelated HSCT; monitor patients for CMV infection/reactivation for 6 months post-transplant regardless of results of donor and recipient pre-transplant CMV serology; consider prophylaxis for CMV infection/reactivation.
Pregnancy and Lactation
- There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to therapy during pregnancy; healthcare professionals are encouraged to register patients and pregnant women are encouraged to enroll themselves by calling 1-877-311-8972.
- There are no adequate and well-controlled studies of use in pregnant women; data on pregnant women are insufficient to inform on drug-associated risk; however, there are clinical considerations for administering live vaccines to infants exposed to the drug while in utero.
- In reproductive toxicology studies in rats and rabbits, no fetal malformations were observed with intravenous administration during organogenesis at doses that produced exposures approximately 29 times the exposure at the maximum recommended human dose (MRHD) of 10 mg/kg/month on an AUC basis; however, in a pre-and postnatal development study in rats, therapy altered immune function in female rats at 11 times the MRHD on an AUC basis.
- It is unknown if abatacept can cross the placenta into the fetus when a woman is treated during pregnancy; the drug is an immunomodulatory agent; it is unknown if the immune response of an infant who was exposed in utero to abatacept and subsequently administered a live vaccine is impacted; risks and benefits should be considered before vaccinating such infants.
Lactation
There is no information regarding the presence of abatacept in human milk. Effects on the breastfed infant, or effects on milk production; however, abatacept was present in the milk of lactating rats dosed with abatacept.
Therapeutic class
DMARDs, Immunomodulators.
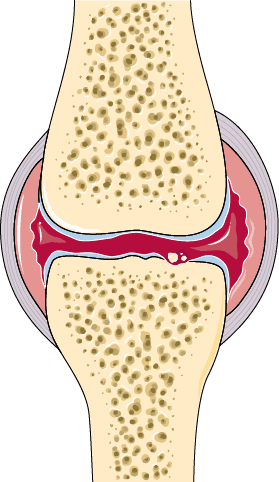
Drug mode of action
Abatacept is a selective co- stimulation modulator – like CTLA-4, the drug has shown to inhibit T-cell (T lymphocyte) activation by binding to CD80 and CD86, thereby blocking interaction with CD28. Blockade of this interaction has been shown to inhibit the delivery of the second co-stimulatory signal required for optimal activation of T-cells. This results in the inhibition of autoimmune T-Cell activation that has been implicated in the pathogenesis of rheumatoid arthritis.
Drug Interaction
If your medical doctor is using this medicine to treat your pain, your doctor or pharmacist may already be aware of any possible drug interactions and may be monitoring you for them. Do not start, stop, or change the dosage of any medicine before checking with your doctor, health care provider, or pharmacist first.
Abatacept has severe interactions with the following drug:
Upadacitinib
Abatacept has serious interactions with the following drugs:
Adalimumab, adenovirus types 4 and 7 live, oral, anakinra, axicabtagene ciloleucel, baricitinib, brexucabtagene autoleucel, certolizumab pegol, ciltacabtagene autoleucel, etanercept, idecabtagene vicleucel, infliximab, influenza virus vaccine quadrivalent, adjuvanted, influenza virus vaccine trivalent, adjuvanted, lisocabtagene maraleucel, tisagenlecleucel, tocilizumab, tofacitinib.
Abatacept has moderate interactions with the following drugs:
Belatacept, cholera vaccine, dengue vaccine, denosumab, fingolimod, hydroxyurea, isavuconazonium sulfate, meningococcal group B vaccine, ocrelizumab, ofatumumab SC, Olaparib, ozanimod, ponesimod, Siponimod, sipuleucel-T, trastuzumab, trastuzumab deruxtecan.
Abatacept has minor interactions with no other drugs.
This information does not contain all possible interactions or adverse effects.
Therefore, before using this product, tell your doctor or pharmacist about all the products you use. Keep a list of all your medications with you and share this information with your doctor and pharmacist. Check with your health care professional or doctor for additional medical advice, or if you have health questions or concern.
Learn more about Genetic medicine click below link





I’d have to examine with you here. Which is not one thing I usually do! I take pleasure in reading a post that may make folks think. Additionally, thanks for permitting me to comment!
Hey, I think your site might be having browser compatibility issues. When I look at your blog in Opera, it looks fine but when opening in Internet Explorer, it has some overlapping. I just wanted to give you a quick heads up! Other then that, fantastic blog!
I simply wished to appreciate you all over again. I do not know the things I would’ve used without the type of solutions contributed by you regarding this situation. It actually was the horrifying issue in my position, however , understanding the very expert technique you treated that took me to leap with gladness. I’m just thankful for your service and even pray you realize what a powerful job you are always accomplishing instructing most people via your web page. I am certain you’ve never met any of us.
Awesome blog! Is your theme custom made or did you download it from somewhere? A design like yours with a few simple tweeks would really make my blog stand out. Please let me know where you got your theme. Cheers
Real clean internet site, appreciate it for this post.
Touche. Solid arguments. Keep up the amazing spirit.
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article.
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
The point of view of your article has taught me a lot, and I already know how to improve the paper on gate.oi, thank you.
I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article.
I am not sure where you’re getting your info, but great topic. I needs to spend some time learning more or understanding more. Thanks for fantastic info I was looking for this information for my mission.
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
Thanks for sharing. I read many of your blog posts, cool, your blog is very good.
I’d have to examine with you here. Which is not one thing I usually do! I take pleasure in reading a post that may make folks think. Additionally, thanks for permitting me to comment!
F*ckin¦ remarkable things here. I¦m very happy to see your post. Thank you a lot and i’m having a look ahead to contact you. Will you please drop me a mail?
I got good info from your blog
I am extremely impressed along with your writing talents and also with the structure on your blog. Is this a paid subject matter or did you modify it your self? Anyway stay up the nice high quality writing, it’s uncommon to peer a nice blog like this one today..
Excellent blog here! Also your web site loads up very fast! What host are you using? Can I get your affiliate link to your host? I wish my site loaded up as fast as yours lol
Fantastic job breaking down this topic, like a demolition crew for my misconceptions.
I am continuously browsing online for posts that can assist me. Thanks!
Thanks for another informative blog. Where else could I get that type of information written in such an ideal way? I’ve a project that I am just now working on, and I have been on the look out for such information.
This post has been incredibly helpful to me. The guidance is something I’m truly grateful for.
The arguments were as compelling as The online persona. I’m totally sold—and not just on The ideas.
I loved The fresh take on this topic. The points resonated with me deeply.
Your article helped me a lot, is there any more related content? Thanks!